Winston, OR – April 7, 2025
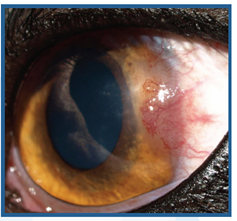
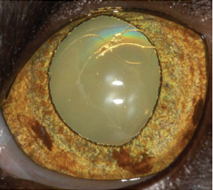
Wildlife Safari is pleased to announce that renowned veterinary ophthalmologist Dr. Cassandra Bliss, of Bliss Animal Eye Care in Medford, OR, has achieved a remarkable milestone—successfully performing cataract surgery on two female African lions in a single day. The lionesses, Serafina and Mtai, were recently diagnosed with cataracts by Dr. Bliss following the initial discovery of cloudiness developing in each of their right eyes by the park’s dedicated carnivore team and veterinary staff. Cataracts can cause blurred vision and sensitivity to light, and the surgery helps restore clear sight.
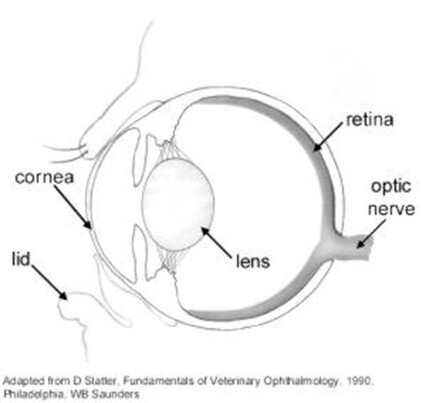
Dr. Bliss, a trusted partner of Wildlife Safari since 2014, has provided expert care for a variety of species at the park—including bears, cheetahs, lions, flamingos, and lemurs. Serafina and Mtai began to lose their sight, Dr. Bliss determined that cataract surgery was necessary to save their vision. This procedure involves removing the cloudy lens—the cataract—and replacing it with a clear artificial one. To do this, Dr. Bliss used a technique called phacoemulsification, which uses ultrasonic energy to break up the cataract, creating space for the new artificial lens to be placed.
Performing cataract surgery on lions is no small task—it takes steady hands, sharp eyes, and a team of experts- especially to perform surgeries on two lions in one day. To ensure the procedure caused minimal disruption to the animals, Dr. Bliss assembled a specialized team of veterinary experts and surgical equipment professionals from across the country. She was joined by Dr. Paige Evans, a veterinary ophthalmologist from Florida; Dr. Benji Alcantar, Wildlife Safari’s head veterinarian, and his staff, and the staff of Bliss Animal Eye Care. Representatives from Prescott’s Inc. carefully disassembled and transported Dr. Bliss’s specialized Zeiss surgical microscope—a vital tool for the delicate procedure to the sanctuary’s surgical suite. The custom lenses, based on precise preoperative measurements, were crafted by An-Vision in Hennigsdorf, Germany, while the ultrasonic surgical tool for the phacoemulsification was supplied by the Swiss company Oertli.
“The surgery was a great success,” said Wildlife Safari’s Head Veterinarian, Dr. Benji Alcantar. “We are still closely monitoring the lions' recovery, but the procedure itself went perfectly.” As of today, Dr. Bliss and Wildlife Safaris are pleased to announce that Serafina and Mtai have made a full recovery with improved vision and a better quality of life.